DATE: 12TH OF JULY, 2025
- INTRODUCTION
On July 12th, 2025, a joint free medical outreach was conducted by the National Association of Seadogs, Abuja (Sahara and Zuma deck) at Kukwaba Village, situated within the Kubwa district of Bwari Area Council, Federal Capital Territory (FCT), Abuja. This intervention was organised as part of a broader humanitarian effort to provide accessible healthcare services to underserved and peri-urban populations in the FCT.
Kukwaba is a semi-urban settlement located approximately 5 kilometres from the Abuja city centre. It lies within one of the most rapidly urbanising and densely populated districts in the territory—Kubwa—whose population has grown significantly since the 1980s due to internal resettlement and migration. Although specific population data for Kukwaba is unavailable, its proximity to major urban growth corridors suggests a substantial and growing community with limited access to structured primary healthcare services.
Environmental and public health studies in the Kubwa district, including Kukwaba, have documented close human-animal proximity, especially due to unregulated backyard poultry farming. This has raised public health concerns regarding zoonotic disease transmission, in addition to noise and environmental pollution. These local risk factors, compounded by socio-economic challenges, have contributed to the community’s vulnerability to communicable diseases such as malaria, respiratory infections, and gastrointestinal illnesses—ailments that mirror the broader disease burden observed across FCT’s area councils.
The medical mission sought to address these needs by providing essential medical services, health education, basic laboratory investigations, and referrals where necessary. This report summarises the objectives, activities, findings, challenges, and recommendations derived from the outreach.
2. OBJECTIVES OF THE MEDICAL MISSION
– To provide basic healthcare services to underserved residents of Kukwaba Village.
– To offer clinical consultations, laboratory services, and free drug dispensation.
– To raise awareness about hygiene, nutrition, and common preventable diseases.
– To identify cases that require urgent referrals to secondary or tertiary healthcare facilities.
- TEAM COMPOSITION
The medical team comprised:
– 5 Medical doctors
– 2 Medical laboratory scientists
– 4 Pharmacists
– Volunteers and support teams, and members of the National Association of Seadogs
- DEMOGRAPHICS OF BENEFICIARIES
A total of 237 forms were recorded, standing as our total population; 234 out of the 237 were attended to about consultations, and 224 followed through and were registered for diagnosis.
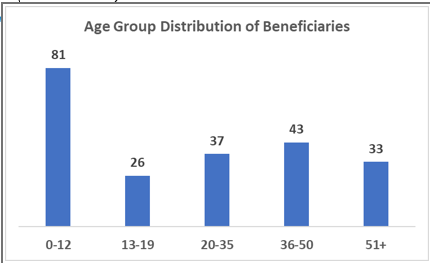
| Figure 1: Age Group Distribution of NAS Medical Mission Beneficiaries (n = 220) |
The chart illustrates the distribution of NAS Medical Mission beneficiaries across five age groups.
The largest proportions of beneficiaries were children aged 0–12, accounting for 81 individuals (37.9%), highlighting a strong focus on paediatric care in the communities served.
Beneficiaries in the 36–50 age group followed, with 43 individuals (20.1%), and those in the 20–35 age group contributed 37 beneficiaries (17.3%), demonstrating substantial engagement of middle-aged and young adults.
Older adults aged 51 and above represented 33 individuals (15.4%), while adolescents aged 13–19 made up the smallest group, with 26 individuals (12.2%).
These findings indicate that while children are the most served group, the mission also reaches a significant number of adults and older adults, underscoring the need for a balanced approach that addresses health needs across all age categories.
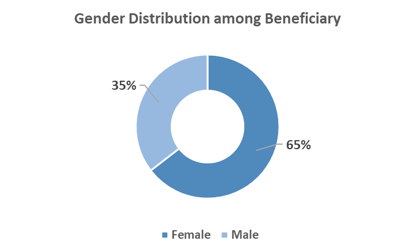
| Figure 2: Gender Distribution of Beneficiaries of Kukwaba Mission (n=220) |
The chart illustrates the gender distribution of beneficiaries reached by the NAS Medical Mission. Of the total beneficiaries, 65% (n=142) were female, while 35% (n=78) were male.
This notable predominance of female beneficiaries suggests that the medical mission services may particularly resonate with, or meet more immediate health needs of, women in the communities served. It could also reflect the greater health-seeking behaviour observed among women compared to men, or targeted services that are more relevant to women.
Further exploration might help understand whether the higher female turnout is driven by the nature of services offered, community dynamics, or accessibility factors, and whether additional strategies are needed to engage more male beneficiaries.
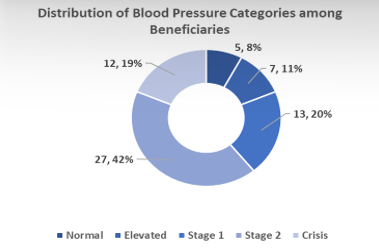
| Figure 3: Distribution of Blood Pressure Categories among NAS Medical Mission Patients (n = 64) | Figure 4: Distribution of Blood Pressure Classifications by Gender among NAS MM Beneficiaries (n = 64) |
The Blood Pressure (BP) readings of sixty-four (64) beneficiaries were taken. Figure 3 illustrates the distribution of (BP) readings among patients screened during the NAS Medical Mission. A total of 64 patients had their BP measured and classified according to the American Heart Association (AHA) criteria.
- Normal BP was observed in 8% (5 patients) of the participants, indicating optimal cardiovascular health.
- Elevated BP was detected in 11% (7 patients), suggesting early signs of risk that may require lifestyle modifications.
- Stage 1 Hypertension was recorded in 20% (13 patients), warranting closer monitoring and possible medical advice.
- Stage 2 Hypertension was the most prevalent category, seen in 42% (27 patients), reflecting a significant burden of high blood pressure among the community served.
- Alarmingly, 19% (12 patients) were in a Hypertensive Crisis, which indicates dangerously high BP levels requiring immediate medical attention.
These findings underscore the critical need for ongoing hypertension screening, awareness, and management interventions in the target population to reduce the risk of cardiovascular complications.
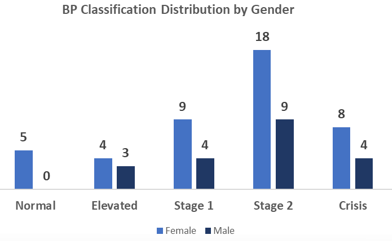
Figure 4 illustrates the distribution of blood pressure (BP) classifications across gender among the NAS Medical Mission (NAS MM) beneficiaries.
- The majority of both females and males fell into the Stage 2 hypertension category, with 18 females and 9 males, indicating a high prevalence of severe hypertension.
- A notable proportion of females (8) and males (4) were also in the Crisis BP category, highlighting the urgency for medical intervention in these cases.
- Stage 1 hypertension was more common in females (9) than males (4), while Elevated BP affected 4 females and 3 males.
- Only 5 females recorded Normal BP, and no male beneficiaries fell into this category.
These findings suggest that elevated and hypertensive BP levels are prevalent among both genders, with females showing higher frequencies across all categories except for Stage 2 and Crisis, where males also showed significant numbers. The results emphasize the need for targeted interventions and follow-up care, particularly for those in the higher BP categories.
Table 1: Blood Pressure Classification by Age Group and Sex (n = 64)
| Age Group | Sex | Crisis | Elevated | Normal | Stage 1 | Stage 2 | Total |
| 0-19 | Female | 1 | 0 | 0 | 1 | 0 | 2 |
| 20-35 | Female | 0 | 1 | 2 | 2 | 4 | 9 |
| 20-35 | Male | 0 | 1 | 0 | 1 | 2 | 4 |
| 36-50 | Female | 3 | 1 | 3 | 4 | 7 | 18 |
| 36-50 | Male | 2 | 1 | 0 | 2 | 3 | 8 |
| 51+ | Female | 4 | 2 | 0 | 2 | 7 | 15 |
| 51+ | Male | 2 | 1 | 0 | 1 | 4 | 8 |
| Total | 12 | 7 | 5 | 13 | 27 | 64 |
This analysis examines the distribution of blood pressure (BP) classifications among beneficiaries, cross-tabulated by age group and sex. The findings provide a clearer understanding of the prevalence of hypertension and normotension across demographic segments.
The results reveal distinct patterns:
- Sex differences: Females are more represented in the dataset and also have higher counts across most BP categories. Notably, more females appear in the Stage 2 Hypertension and Crisis categories compared to males. This could reflect either a higher prevalence of elevated BP among women in this population, or simply their larger representation among beneficiaries.
- Age group trends:
- Among younger age groups (19–35), the majority fall within Normal, Elevated, or Stage 1 Hypertension categories, with few progressing to Stage 2 or Crisis.
- In the middle-aged (36–50), there is an increase in Stage 2 Hypertension, indicating higher cardiovascular risk emerging in this group.
- For older age groups (51–65 and above), Stage 2 Hypertension and Crisis-level BP readings become more frequent, particularly among females.
- Critical concern: The presence of individuals in the Hypertensive Crisis category across age groups, including some younger adults, signals an urgent need for follow-up care and hypertension management in the community.
Implications
The findings highlight the importance of age- and sex-sensitive health education, targeted screening, and intervention programs. Efforts should focus on:
- Early detection in younger adults to prevent progression.
- Tailored interventions for middle-aged and older adults who show higher prevalence of advanced hypertension stages.
- Strengthening outreach and follow-up, especially for women who seem to exhibit higher rates of severe hypertension in this sample.
Summary of Diagnoses
Table 2: Top Diagnoses (by count & % of total) (n = 220)
| Condition | Count | Percentage |
| Helminthiasis | 73 | 32% |
| Malaria | 56 | 24% |
| Hypertension (HTN/High BP) | 19 | 8% |
| Peptic Ulcer Disease (PUD) | 17 | 7% |
| Upper Respiratory Tract Infection (URTI) | 10 | 4% |
| Gastritis | 8 | 3% |
| Arthritis | 4 | 2% |
| Myalgia | 3 | 1% |
| Others (e.g., allergy, stress, fever, eye issues, benign mass, menorrhagia, etc.) | 37 | 16% |
| Stable health condition | 12 | 5% |
Comorbid Conditions
Total beneficiaries with more than one condition (comorbid): ~82 (~36% of total).
Common comorbidity patterns:
- Malaria + HTN
- Malaria + PUD
- Helminthiasis + Malaria
- HTN + Arthritis
- URTI + Helminthiasis
- Malaria + Gastritis
- Helminthiasis is the most frequently diagnosed condition, accounting for nearly one-third of all diagnoses, likely reflecting endemic parasitic infections in the area.
- Malaria remains a significant burden, found in about a quarter of beneficiaries.
- A considerable proportion of beneficiaries (~36%) presented with comorbid conditions, underscoring the need for integrated care rather than single-disease management.
- Chronic conditions like hypertension, arthritis, and PUD also appeared often, sometimes in combination with infectious diseases like malaria, highlighting the double burden of communicable and non-communicable diseases.
Table 3: Summary of Drugs Dispensed
| Drug / Category | Examples / Notes | Prevalence |
| Antihypertensives | Amlodipine, Lisinopril, Nifedipine, Vasoprin | Frequent |
| Antimalarials (ACT) | ACT (Artemisinin Combination Therapy), AL (Artemether-Lumefantrine) | Very frequent |
| Analgesics / Antipyretics | Paracetamol (PCM), Ibuprofen, Diclofenac | Very frequent |
| Anthelmintics (Deworming) | Albendazole, Albendazole syrup, “Alberodyl” | Very frequent |
| Gastroprotective agents | Omeprazole, Antacids, Gestid | Frequent |
| Antibiotics | Amoxicillin, Ciprofloxacin, Metronidazole (Flagyl), Septrin | Frequent |
| Vitamins & Supplements | Multivitamins, Vitamin C, Folic Acid, Ferobin | Frequent |
| Antihistamines & Steroids | Loratadine, Piriton (Chlorpheniramine), Hydrocortisone cream | Common |
| Cough and Cold Remedies | Cough syrups, Funbact A (topical) | Common |
| Others | Mycotem, Fluconazole, Glimepiride, Metformin (diabetes), Zinc, ORS | Less frequent |
- KEY FINDINGS / OBSERVATIONS:
The analysis of medications dispensed during the NAS Medical Mission highlights a strategic focus on addressing the dual burden of infectious and chronic diseases among beneficiaries. The most frequently administered medications were antimalarials (ACT), reflecting the high prevalence of malaria, and anthelmintics (Albendazole), aligned with the significant occurrence of helminthiasis.
Analgesics and antipyretics (PCM, Ibuprofen) were also common, providing symptomatic relief.
A considerable number of patients received antihypertensives (Amlodipine, Lisinopril), underscoring the importance of addressing non-communicable diseases alongside acute infections.
Vitamins and supplements were widely given as supportive therapy, while antibiotics and antihistamines targeted specific infections and allergic reactions.
The presence of multi-drug regimens reflects the reality of comorbid conditions within the population.
- RECOMMENDATIONS
Based on data analysis and identified health trends, the following recommendations are proposed:
Short-term Interventions:
- Malaria Prevention Campaign: Distribute insecticide-treated bed nets and conduct community education on environmental management to reduce mosquito breeding sites.
- Follow-up Care Program: Establish a mechanism to ensure patients with chronic conditions (hypertension, diabetes) receive continued care and medication.
- Respiratory Health Initiative: Provide education on preventing respiratory infections and improving indoor air quality.
- Women’s Health Clinic: Organise a dedicated follow-up clinic focusing on reproductive health issues identified during the outreach.
Medium-term Interventions:
- Community Health Workers Program: Train community health workers to provide basic health education, monitor chronic conditions, and facilitate referrals.
- Regular Health Screening: Implement quarterly health screening for non-communicable diseases, particularly hypertension and diabetes.
- School Health Program: Develop a comprehensive health program for schools in the community, focusing on deworming, nutrition, and respiratory health.
Long-term Strategies:
- Community Health Centre: Advocate for the establishment of a permanent primary healthcare centre within the community.
- Health Insurance Scheme: Work with stakeholders to develop a community-based health insurance scheme to improve financial access to healthcare.
- Environmental Health Projects: Partner with environmental agencies to address underlying environmental factors contributing to disease burden.
- Comprehensive Data System: Establish a community health information system to track health trends and evaluate interventions over time.
- Encourage partnerships with local health authorities, relevant key stakeholders in the community, the local government agency, and the office of the FCT minister.
- CONCLUSION:
The Kukwaba Village medical mission addressed critical healthcare needs and provided relief to a vulnerable population. The turnout and reception by the community underscore the importance of continued intervention in similar underserved regions. Collaboration with stakeholders and improved planning can further enhance the reach and sustainability of such missions.
https://www.facebook.com/share/p/1ALZknvsAW/
https://x.com/NASPC1952/status/1945178897194115143?t=tibnOKVyedGWwqTnG8XIfQ&s=08
https://youtu.be/UMY2CrLz9eA?si=Ddl68fJVgCYzJESx
https://www.facebook.com/share/v/16X2gJGoL7/?mibextid=xfxF2i
https://youtu.be/8-v3gmyTVIw?si=UEju7QglRoGt-cZ8